Total Shoulder Arthroplasty

Christopher Shultz, MD
We are in this together!
We want your recovery to be as pain free and pleasant as possible. Please read these instructions before surgery to prepare you for what to expect.
The shoulder is a ball and socket joint that enables you to raise, twist, bend and move your arms forward, to the sides and behind you. The head of the upper arm bone (humerus) is the ball and a circular depression (glenoid) in the shoulder bone (scapula) is the socket. The head of the upper arm bone is coated with a smooth, durable, covering (articular cartilage) and the joint has a thin, inner lining (synovium) for smooth movement. The surrounding muscles and tendons provide stability and support.
In an arthritic shoulder the normal cartilage is worn away and there is bone-on-bone without the normal smooth gliding surfaces which are able to glide on one another with little friction and wear. The joint may also become irregular from bony growth (osteophytes) which is the body’s attempt to “heal” the cartilage injury. Pain is usually due to the irregular joint surfaces rubbing on one another and from the inflammation of this wear and tear.
Many people know someone with an artificial knee or hip joint. Less common, but just as successful in relieving joint pain is a shoulder replacement (arthroplasty). Conventional shoulder replacement surgery replaces damaged joint surfaces with artificial parts (prostheses). There are two components: The humeral component replaces the head of the upper arm bone, while the glenoid component replaces the socket (the glenoid depression).
This type of shoulder replacement requires intact rotator cuff tendons. These are tendons which encircle the humeral head (ball) and help to keep the humeral head in the glenoid (socket) when the arm is elevated. These tendons also help to rotate the humerus on the glenoid so the arm can be raised. Without normal function of the rotator cuff the humeral head may move upward out of the glenoid socket and it is then difficult or impossible to raise the arm up. The front rotator cuff tendon (subscapularis) is detached to allow placement of the shoulder replacement. This tendon is then reattached at the end of the surgery. To protect this tendon repair, you should not rotate your shoulder away from your body (external rotation) for the first 6 weeks after surgery.
This shoulder implant has been used in Europe and the United States since the 1990’s. While the experience has been very successful, complications have been reported. Most patients report minimal or no pain after surgery and most are able to raise the arm much higher than before surgery.
Complications can include the following:
- Infection
- Instability of the joint replacement
- Fracture of either the humerus or glenoid bone
- Nerve injury
- Exacerbation of underlying carpal tunnel
- Loosening of the joint replacement
- Failure of the rotator cuff tendons
- Anesthesia problems
- Hematoma or blood clots
Preparation for Surgery
Shoulder replacement surgery is routine, but should still be considered a major surgery.
Support: We recommend you arrange to have a family member or friend stay with you for minimum 2 to 3 days after surgery to help you adjust to the recovery process.
Meals: Arranging meals or pre-making frozen meals can be very helpful.
Sleep: Sleeping can often be uncomfortable and challenging for the first several weeks after surgery. Many patients prefer to sleep in a recliner or partially upright on a couch.
Day Surgery vs. Overnight Stay
Shoulder replacement surgery can be performed safely as an outpatient procedure (go home same day). Most patients prefer to recover in the comfort of their own home and do not need to stay the night after surgery. You will be monitored closely in the recovery area right after surgery to ensure you are safe before being discharged home. In some cases your surgeon will recommend an overnight stay based on your individual medical needs and medical conditions.
Post Operative Instructions
- Mobility: Move! Move! Move! Our bodies were meant to move and generally feel better when we are more active. Your shoulder mobility will be limited by a sling, but you should still walk 3 to 4 times a day for minimum 10 minutes.
- Sling: you will be discharged with a sling and wedge pillow after surgery. You should expect to wear the sling at all times for the first two weeks. After two weeks, you can take the sling off at home, but should continue to wear it when sleeping and when out in public (to remind others that you had surgery).
- During the first 4 weeks you should avoid active internal rotation of your shoulder to protect the rotator cuff tendon repair.
- Pain: Pain after surgery is normal. Most patients will have a nerve block just prior to surgery to decrease pain after surgery. This typically lasts 24 hours. As the pain block wears off, we will utilize multiple strategies to decrease your pain and improve your comfort after surgery. The goal is to minimize opioid medication’s, which are addictive and dangerous.
Utilizing these strategies, most patients will not need more than one or two days of opioid pain medication following surgery:
- PolarCare ice pack provides ice water cooling to help reduce swelling and pain. Use it continuously for 3 days as long as skin is protected from direct contact with the pad.
- Tylenol 500 mg (acetaminophen extra strength) – Take 2 tablets every 8 hours on a scheduled basis for the first 2 weeks after surgery, even if you are not having pain. Do not exceed 3,000 mg/day. After 2 weeks, you may take it only as needed.
- Naproxen 500 mg (or over-the-counter Aleve 220 mg, take 2 pills)– Take this twice a day with food, first dose with breakfast and second dose with dinner. You may discontinue this medication when you are no longer experiencing pain and not requiring the use of prescription pain medicine. If you experience any stomach discomfort or pain, discontinue this medication. Pepcid or Prilosec over-the-counter medications can be taken to protect your stomach if you have discomfort.
- Oxycodone 5mg. Opioids are narcotics and are addictive. It is best to limit the use of opioids as much as possible for pain. The other medications you are prescribed will help limit your need for opioids. Take as directed on an as needed basis every 3-4 hours. Narcotic pain medicine can only be filled during regular office hours and not on nights or weekends so please do not call the office for refills at this time.
- Colace (Over-the-counter) If you do develop constipation you may take an over the counter stool softener such as 100 mg by mouth twice daily.
- Zofran 4 mg– (optional) Take 1 tablet every 6 hours as needed for nausea. It is not uncommon to develop nausea after surgery or from taking narcotic pain medication. However, if you do not have problems with nausea while taking pain medications you do not need to fill this prescription.
- Blood Clot Prevention: Blood clots following surgery are rare, but can be catastrophic if they occur. The best prevention is maintaining mobility and limiting sedentary activities. To reduce your risk, we will prescribe you an 81mg baby aspirin to take twice a day. Take this for the first two weeks following surgery.
- Dressings & Wound Care: You will be discharged with a waterproof dressing. Starting on postoperative day 3 it is OK to shower and let water run over the dressing. You will be given an extra, lighter sling to wear in the shower. This can be dried in the dryer after showering. If your dressing comes loose or gets wet, simply remove the dressing and pat the wound dry. Replace the dressing with a clean over the counter dressing from CVS or Walgreens.
Some dressings will become saturated from body fluid following surgery. Do NOT be alarmed. Simply reinforce the dressing with a gauze pad and tape. If any redness, increased swelling, pus-like drainage, fever > 101o F or increasing pain develops, please call the office. After the staples/sutures have been removed, the wounds will be very sensitive to the touch. The wounds can be desensitized by rubbing them in a circular motion with a hand lotion like Palmer’s contains vitamin E and cocoa butter. This wound program will make for softer and more comfortable scars.
- Swelling: Swelling and bruising along the arm and chest wall is common after surgery. Patient’s on blood thinners (i.e. Plavix, Coumadin) are at higher risk of bruising. Daily exercises to bend and straighten the elbow and squeeze a ball in your hand will help to decrease swelling. Applying gentle warm compress, alternating ice, and keeping the arm elevated all help to resolve the bruising.
- Clothing: Most people wear a shirt or blouse that buttons in the front of the first few weeks. Others use a loose large T-shirt and pull it over the shoulder and sling.
- Driving: You may use your arm to perform normal daily activities, such as eating, writing or shaving, but you may not lift any items or reach out suddenly until you are instructed that it is OK to do so. when you regain full shoulder movement, you can probably resume driving. This usually takes around 2-6 weeks.
Basic Exercises
You should wear your sling full time for the first 4 weeks, and when out of the house or sleeping from weeks 4-6. You should take off your sling at home starting post-operative day 2 and perform the following exercises 3-4 times per day, 10 sets at a time. Make sure you can see your elbow at all times when doing these exercises. Reaching behind your back can cause your shoulder to dislocate.
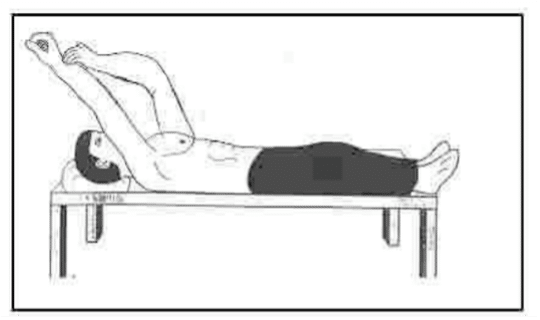
1. Supine forward flexion: Lie on your back. Hold the affected arm at the elbow with the opposite hand. Assisting with the opposite arm, lift the operated arm upward, as if the bring the arm overhead. Slowly lower the arm back to the bed. Repeat 10 times per session.

2. Wall walks: stand with your shoulder about 2 feet from the wall. Raise your arm to shoulder level and gently “walk” your fingers up the wall as high as you can. Hold for a few seconds. Then walk your fingers back down. Repeat 10 times. Move closer to the wall as you repeat. Build up to holding each stretch for 30 seconds.

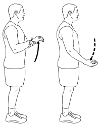
3. Isometric shoulder abduction (the chicken wing): Resisting upward motion to the side, slowly and gently push your arm against the back of chair. Hold for 5 seconds, and then relax. Repeat 10 times per session.
4. Elbow stretch: 3 times per day, remove your sling and let gravity stretch your elbow full straight. Repeat this 10 times per session.
5. Posture: When you no longer need to wear your sling, it is important to stretch your back and shoulders to regain your pre surgery posture. Posture is important especially for a good functioning shoulder. Gently roll your shoulders a few times and squeeze your shoulder blades together. Gently hold this position for 10 seconds.
Sample Daily Calendar for First 2 Weeks Post-op
Proper nutrition and sleep are paramount to healing and managing pain after surgery. A balanced diet with emphasis on lean protein and vegetables should be part of every meal. Our bodies expend nearly twice as many calories recovering from surgery. If needed, supplement your diet with protein shakes to give it the fuel to heal. Minimizing inflammatory foods high in refined sugar will help with recovery and reduce pain. While challenging after shoulder surgery, effort must be taken to get good rest! Limiting screen time and developing a routine schedule of going to bed and waking up are important for good sleep hygiene.
| Time | Activity |
| 7:30 |
Wake up Take Naproxen 500mg, 81mg baby aspirin |
| 7:45 |
Shoulder stretches – remove sling (repeat each 10 times):
|
| 8:15 | Eat a healthy breakfast (think high protein- lean meats, eggs, vegetables) |
| 8:45 | Clean up, take a shower. Use shower sling, then put in dryer |
| 9:30 | Go for a walk outside |
| 10:30 |
Shoulder stretches – remove sling (repeat each 10 times)
|
| 11:30 | Prepare lunch (high protein is key, maintain hydration) |
| 1:30 | Take 2 tablets of Tylenol 650mg |
| 1:45 | Catch up with an old friend over the phone |
| 3:30 |
Shoulder stretches – remove sling (repeat each 10 times)
|
| 5:30 | Prepare dinner (lean meats, high vegetables) |
| 6:30 | Take Naproxen 500mg |
| 7:00 |
Take a stroll around the neighborhood, watch the sunset Take 81mg baby aspirin |
| 7:45 |
Shoulder stretches – remove sling (repeat each 10 times)
|
| 8:30 | Take 2 tablets of Tylenol 650mg |
| 8:45 |
Prepare for bedtime
|
Physical Therapy Protocol
Phase I (surgery to 4 weeks after surgery)
|
Rehabilitation goals
|
Reduce pain and swelling in the shoulder after surgery Maintain active range of motion (AROM) of the elbow, wrist and neck Protect healing of repaired tissues and implanted devices |
|
Precautions
|
Use sling continuously except while doing therapy or light, protected activities – such as desk work, for 4 weeks Wear sling while sleeping for 6 weeks OK for active assist forward flexion No active internal rotation for 6 weeks External rotation range of motion limited to 30 degrees Relative rest to reduce inflammation |
|
Suggested therapeutic exercises
|
Elbow, wrist and neck AROM Ball squeezes Passive and active assistive range of motion (AAROM) for shoulder flexion and abduction to patient tolerance Codmans/Pendulum exercises Pain free isometrics for shoulder flexion, abduction, extension and external rotation |
|
Cardiovascular exercise
|
Walking or stationary bike with sling on No treadmill |
|
Progression criteria |
4 weeks after surgery |
Phase II (begin after meeting Phase I criteria, usually 4-8 weeks after surgery)
|
Rehabilitation goals
|
Controlled restoration of passive and active assistive range of motion Activate shoulder and scapular stabilizers in a protected position of 0 degrees to 30 degrees of shoulder abduction Correct postural dysfunctions |
|
Precautions
|
No lifting anything heavier than a coffee cup Wean out of the sling slowly based on the safety of the environment during weeks 5 and 6. Discontinue use of the sling by the end of week 6 Wear sling while sleeping for 6 weeks No active internal rotation for 6 weeks External rotation range of motion limited to 30 degrees weeks 5 and 6, then to 45 degrees for weeks 7 and 8 |
|
Suggested therapeutic exercises
|
Passive and active assistive range of motion for the shoulder in all cardinal planes Pain free, progressive, low resistance shoulder isotonics Gentle, low velocity rhythmic stabilizations to patient tolerance Scapular strengthening with the arm in neutral Cervical spine and scapular active range of motions Postural exercises Core strengthening |
|
Cardiovascular exercise
|
Walking or stationary bike No treadmill or stair master Avoid running and jumping because of landing impact |
|
Progression criteria |
8 weeks after surgery |
Phase III (begin after meeting Phase II criteria, usually 8 weeks after surgery)
|
Rehabilitation goals
|
Functional shoulder range of motion in all planes Normal (rated 5/5) strength for shoulder internal rotators and external rotators with the shoulder in 0 degrees of abduction Correct any postural dysfunction |
|
Precautions
|
External rotation range of motion limited to 60 degrees No lifting more than 15 pounds |
|
Suggested therapeutic exercises
|
Shoulder internal rotation and external rotation with theraband or weights that begin at 0 degrees of shoulder abduction-gradually increase shoulder abduction as strength improves Open kinetic chain shoulder rhythmic stabilizations in supine (ie. stars or alphabet exercises) Gentle closed kinetic chain shoulder and scapular stabilization drills-wall ball circles and patterns Proprioceptive neuromuscular facilitation patterns Side lying shoulder flexion Scapular strengthening Active, active assistive and passive range of motion at the shoulder as needed Core strengthening Begin trunk and hip mobility exercises |
|
Cardiovascular exercise
|
Walking or stationary bike No treadmill or stair master Avoid running and jumping because of landing impact |
|
Progression criteria |
12 weeks after surgery |
Phase IV (begin after meeting Phase III criteria, usually 12 weeks after surgery)
|
Rehabilitation goals
|
Normal (rated 5/5) rotator cuff strength and endurance at 90 degrees of shoulder abduction and scaption Advance proprioceptive and dynamic neuromuscular control retraining Achieve maximal shoulder external rotation (no limitations) Correct postural dysfunctions with work and sport specific tasks Develop strength and control for movements required for work or sport |
|
Precautions
|
Soreness should go away within 12 hours of activities |
|
Suggested therapeutic exercises
|
Multi-plane shoulder active range of motion with a gradual increase in the velocity of movement while making sure to assess scapular rhythm Shoulder mobilization as needed Rotator cuff strengthening in 90 degrees of shoulder abduction and overhead (beyond 90 degrees of shoulder abduction) Scapular strengthening and dynamic neuromuscular control in open kinetic chain and closed kinetic chain positions Core and lower body strengthening |
|
Cardiovascular exercise
|
Walking, stationary bike or stair master No treadmill or swimming Begin light jogging and running if patient has normal (rated 5/5) rotator cuff strength in neutral and normal shoulder active range of motion |
|
Progression criteria |
Full shoulder active range of motion in all planes and multiplane movements |
Phase V (begin after meeting Phase IV criteria, usually 18 weeks after surgery)
|
Rehabilitation goals
|
Normal strength and endurance of deltoid at 90 degrees of shoulder abduction and scaption Advance proprioceptive and dynamic neuromuscular control retraining Correct postural dysfunctions with work and sport specific tasks Develop strength and control for movements required for work/sport Develop work capacity cardiovascular endurance for work/sport |
|
Precautions
|
None |
|
Suggested therapeutic exercises
|
Multi-plane shoulder active range of motion with a gradual increase in the velocity of movement while making sure to assess scapular rhythm Shoulder mobilization as needed Rotator cuff strengthening in 90 degrees of shoulder abduction as well as in provocative positions and work/sport specific positions, including eccentric strengthening , endurance and velocity specific exercise Scapular strengthening and dynamic neuromuscular control in overhead positions and work/sport specific positions Work and sport specific strengthening Core and lower body strengthening Work specific program, golf program, swimming program or overhead
|
|
Cardiovascular exercise
|
Design to use work/sport specific energy systems |
|
Progression criteria |
May return to sport after receiving surgeon, athletic trainer of PT clearance Return to sport are based on meeting the goals of this phase
|
